Key Points
- MRI shows moderate degenerative changes primarily at L4/L5 and L5/S1 levels, including facet joint arthropathy,
- small disc bulges, and possible contact with descending nerve roots, which may explain ongoing symptoms like pain, numbness, and paresthesia.
- Research suggests these issues can cause radiculopathy, leading to traveling pain, burning, itching, pins and needles,
- and numbness in the lower back and legs, though symptoms vary and may improve with conservative management.
- Weight loss from 107kg to 79kg likely reduces spinal pressure, aiding healing,
- while diet and therapy changes support recovery; evidence leans toward potential full healing without permanent damage if progress continues,
- but monitoring is key.
- Avoiding surgery appears reasonable at this stage,
- as studies indicate many cases resolve with time, physical therapy, and lifestyle adjustments,
- with neurosurgeon estimating 50% healed and another 12 months for further assessment.
- Overview of MRI Findings
- Your recent MRI from September 17, 2025,
- reveals normal structures in the upper lumbar levels
- (T12/L1 to L3/L4), with issues concentrated at L4/L5 and L5/S1.
- These include moderate bilateral facet joint arthropathy
- (wear and tear on the small joints stabilizing the spine)
- combined with small broad-based disc bulges. At L4/L5,
- there’s mild narrowing of the exiting neural foramina
- (openings where nerves exit) without direct compression of exiting roots,
- but possible contact and compression of the descending L5 nerve roots in the subarticular recess (a lateral area in the spinal canal). Similarly, at L5/S1,
- there’s reduced disc signal indicating desiccation (drying out), minor spinal canal narrowing, and contact with descending S1 roots, more on the left.
- The conus medullaris (end of the spinal cord) is normal at L1, with no fractures or major misalignments.
- Explanation of Symptoms and Nerve Involvement
- Symptoms like burning, itching, pins and needles (paresthesia), numbness, and traveling pain often stem from nerve irritation or mild compression, known as radiculopathy.
- In my case, the combination of disc bulges and facet arthropathy at L4/L5 and L5/S1 can irritate the L5 and S1 nerve roots.
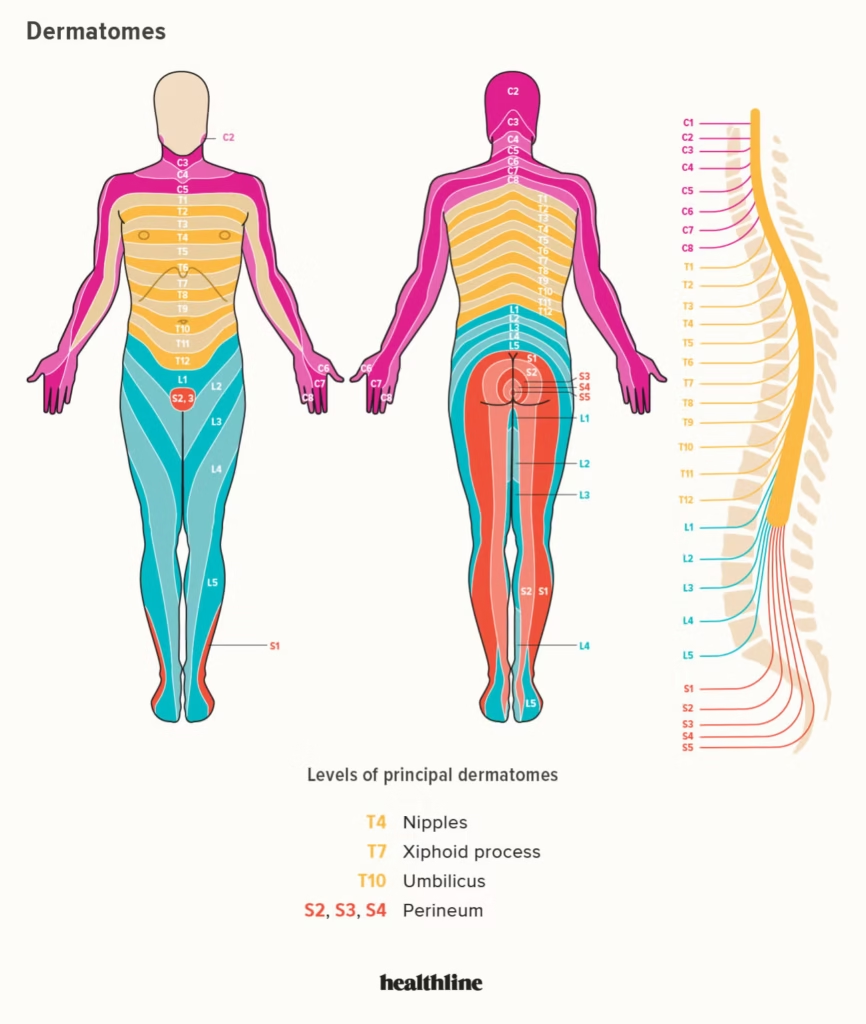
- These nerves supply sensation to specific areas (dermatomes): L5 typically affects the outer calf, top of the foot, and big toe,
- while S1 impacts the outer foot, heel, and little toe. Irritation here can cause pain to radiate from the lower back into the buttocks, thighs, or feet, sometimes
- feeling like a unified pain due to overlapping nerve pathways. The subarticular contact may lead to inflammation, amplifying sensations like burning or itching without full compression.
- Progress, Healing, and Risk of Permanent Damage
- weight loss of 28kg has likely eased pressure on the discs and joints,
- potentially allowing space for healing and reducing inflammationstudies show even modest reductions can relieve 4-10 times the pressure per pound lost. Intermittent fasting may help by lowering inflammation markers,
- though evidence is emerging and should be monitored medically. With pain reduced and neurosurgeon noting 50% healing, continued conservative approaches like physiotherapy and osteopathy
- (now 2 gym sessions and 1 osteopath treatment weekly) support muscle rebuilding and stability.
- Recovery from such nerve issues often takes 6-12 months or more;
- while permanent damage is possible if compression persists long-term, current mild findings and progress suggest it’s avoidable, with reassessment in 12 months to evaluate.
- The lumbar MRI report dated September 17, 2025,
- provides a detailed assessment of my spine, focusing on the lower back region.
- This comprehensive analysis breaks down each section of the report, explains the findings in medical terms supported by anatomical and physiological insights,
- discusses how these issues may interact or “interfere” with adjacent structures, and ties them to the nerve system’s function.
- We’ll also explore how these contribute to my described symptoms
- (e.g., traveling pain, itching, pins and needles, numbness, burning in the lower back),
- the potential for permanent nerve damage, the rationale for avoiding surgery, the benefits of your weight loss and diet strategies, and my reported progress with therapy changes.
- All explanations are grounded in established medical knowledge, with an emphasis on conservative management.
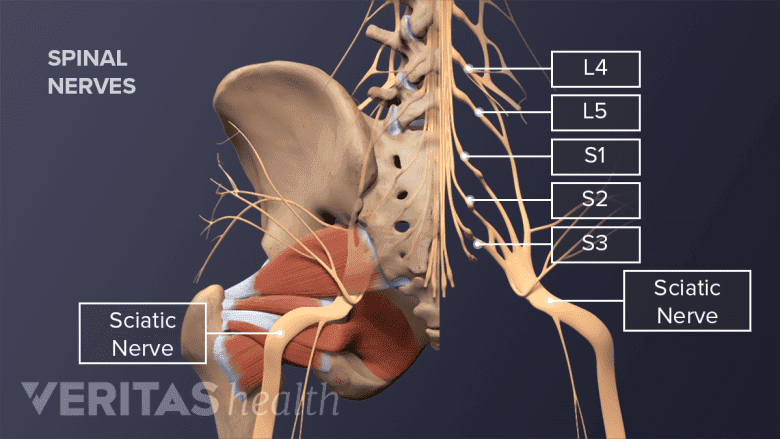
General Anatomy and Nerve System Overview
The lumbar spine consists of five vertebrae (L1 to L5) and the sacrum (S1), - connected by intervertebral discs that act as shock absorbers and facet joints that provide stability and allow movement. Nerve roots exit the spinal canal through foramina (openings) and travel down to form the sciatic nerve and other branches, supplying sensation and motor function to the lower body. Dermatomes are skin areas innervated by specific nerve roots; myotomes are muscle groups controlled by them.
- Compression or irritation (radiculopathy) disrupts signals,
- causing pain that “combines”
- into radiating symptoms as nerves converge in pathways like the lumbosacral plexus. For instance,
- L5 and S1 roots often overlap, leading to unified pain from the back to the foot.
Nerve Root
Dermatome Distribution (Sensory Areas)
Common Symptoms from Irritation
Myotome (Muscle Groups Affected)
L4
Inner thigh, knee, inner calf, top of foot
Pain/numbness in knee/inner leg, weakness in knee extension
Quadriceps (knee extension), tibialis anterior (foot dorsiflexion)
L5
Outer thigh, outer calf, top of foot, big toe
Burning/pins and needles in outer leg/foot, foot drop
Extensor hallucis longus (big toe extension), peroneals (foot eversion)
S1
Buttocks, back of thigh/calf, outer foot, little toe
Aching/burning in heel/sole, difficulty standing on toes
Gastrocnemius/soleus (plantarflexion), hamstrings (knee flexion) - This table illustrates how irritation at L4/L5 (affecting L5 root) and L5/S1 (affecting S1 root) can produce your symptoms, with pain traveling due to nerve convergence.
- Detailed Breakdown of MRI Sections
- The report is structured by spinal levels, starting from general findings and progressing caudally (downward). Upper levels are normal, while lower ones show degenerative changes. “Interference” refers to how one abnormality exacerbates another, e.g., a disc bulge combining with facet arthropathy to narrow spaces and irritate nerves.
- General Findings (Vertebral Bodies, Conus, Alignment, Signal): The spine has an “S lumbar type” configuration (normal curvature with L5/S1 as the last disc). Vertebral bodies are normal without fractures or lesions, alignment is straight, and bone signal is uniform (no marrow abnormalities). The conus medullaris ends normally at L1, appearing healthy. No major issues here interfere with lower sections, but overall stability supports the degenerative changes below. This rules out severe systemic problems like tumors or infections, focusing symptoms on mechanical issues.
- T12/L1 to L2/L3 Levels: Normal disc height, signal, and no bulges or narrowing of the spinal canal/foramina. These levels are unremarkable, meaning they don’t contribute to symptoms or interfere with others. They provide a baseline for comparison, highlighting that your issues are localized lower down, where weight-bearing stress is higher.
- L3/L4 Level: Normal disc height/signal, no large bulge, but mild bilateral facet joint arthropathy (degenerative arthritis causing joint enlargement). This causes minimal foraminal narrowing without nerve compression. Interference: Early arthropathy here may add to cumulative stress on adjacent L4/L5, potentially worsening downstream instability, though minimal impact currently. No direct symptoms from this level alone.
- L4/L5 Level: Normal disc height/signal, very small broad-based disc bulge (annulus fibrosus extends outward symmetrically, intact but protruding). Moderate bilateral facet arthropathy, combining to mildly narrow exiting foramina. No exiting root compression, but contact/possible compression of descending L5 roots in the subarticular recess (lateral canal area). Interference: The bulge and arthropathy synergize to encroach on the recess, irritating L5 roots as they descend before exiting at L5/S1. This can amplify symptoms by inflaming nerves, leading to radiculopathy. Facet changes may stem from prior L4/L5 facet issues noted in history, creating a cycle of joint wear and disc stress.
- L5/S1 Level: Reduced disc signal (desiccation, loss of hydration indicating degeneration), very small broad-based bulge, moderate bilateral facet arthropathy. This causes minor canal/foraminal narrowing without exiting root compression, but contact/irritation of descending S1 roots in the subarticular recess (left > right). Interference: Desiccation weakens the disc, making it prone to bulging, which with arthropathy narrows spaces and irritates S1 roots. This level interferes with L4/L5 by compounding nerve stress—L5 roots pass here too—potentially unifying pain as irritated roots converge into the sciatic nerve. History of left S1 paraesthesia aligns with left-sided emphasis.
- Other Structures (Paraspinal Muscles, Kidneys, Aorta): All normal, no lymphadenopathy. This confirms no secondary issues like muscle atrophy or vascular problems interfering with spinal findings. Muscle normality supports your therapy for rebuilding strength.
- Conclusion: Emphasizes moderate arthropathy at L4/L5 with bulge and possible L5 root compression, similar at L5/S1 with S1 root contact.
- This synthesizes how combined pathologies cause symptoms without severe stenosis.
- How the Nerve System Works and Combines into Symptoms
- Nerves in the lumbar spine exit via foramina and descend in the canal before branching.
- At L4/L5, the L5 root descends in the subarticular recess; at L5/S1, the S1 root does similarly.
- Bulges/arthropathy can cause mechanical contact,
- leading to inflammation (chemical radiculopathy) or mild compression.
- This disrupts sensory signals, causing paresthesia
- (itching, pins/needles, numbness) and nociceptive pain (burning). Pain “travels” because roots form plexuses
- e.g., L4-S3 form sciaticawhere irritation at one level affects distal areas. Over 14 months,
- chronic irritation may sensitize nerves (central sensitization), making pain feel unified or widespread.
- My left-sided history suggests asymmetric involvement.
- Possible Permanent Nerve Damage
- Chronic compression risks axonal damage
- (permanent if severe),
- but my mild findings (contact, not full compression)
- suggest neuropraxia (temporary conduction block).
- Recovery can take 6-18 months; studies show 85% resolve in 8-12 weeks conservatively,
- but prolonged cases (like mine) may need up to 2 years.
- Signs of permanence: persistent weakness, atrophy, or unresolving numbness.
- My progress (pain reduced, 50% healed) indicates low risk, but reassess in 12 months as advised.
- Avoiding Surgery and Conservative Management
- Surgery is reserved for severe, unresponsive cases or emergencies
- (e.g., cauda equina).
- My mild changes and improvement support avoidance; trials show conservative treatment
- (PT, weight loss)
- equals surgery outcomes at 1 year for sciatica.
- My shift to 2 physio gym sessions (strengthening core/legs)
- and 1 osteopath (manipulation for joint mobility)
- aids stability, reducing bulge stress.
- Exercises like ADIM or sling training target facets/discs.
- Benefits of Weight Loss and Diet
- Dropping from 107kg to 79kg (1kg/week)
- reduces axial load—each kg lost eases ~4-10kg pressure on discs/joints,
- improving posture, decreasing inflammation, and enhancing mobility.
- This gives “room to heal” by lessening bulge protrusion and arthropathy stress.
- My 3-day fast/small meal cycle (intermittent fasting) may reduce inflammation via autophagy and cytokine lowering,
- supported by studies on chronic pain, though consult a doctor for sustainability.
- Overall Progress and Outlook
- Since March 2025, My strategies have reduced pain severity, aligning with neurosurgeon’s 50% healing estimate.
- Continued weight loss, “flushing” via diet, and therapy rebuild muscles, potentially leading to full recovery in 12 months. Monitor for worsening; if stable, evidence suggests good prognosis without permanence.
- Key Citations
- Making sense of MRI of the lumbar spine – RACGP
- Lumbar Disc Herniation – The Radiology Assistant
- Radiculopathy: Symptoms, Causes & Treatment – Cleveland Clinic
- Dermatomes: What They Are & Locations – Cleveland Clinic
- Conservative Treatment Versus Surgery for Lumbosacral Radiculopathy
- How Weight Loss Can Improve Spine Health
- Intermittent Fasting: Potential Utility in the Treatment of Chronic Pain
- Facet Arthropathy Causes, Symptoms & Treatments
- Lumbar Facet Arthropathy – StatPearls
- Understanding Common Spine Terminology on MRI
- L4-L5 Disc Bulge & Disc Herniation
- Lumbar Disc Degenerative Disease
- What Are the Symptoms of L5-S1 Nerve Damage?
- Lumbar Radiculopathy – Symptoms, Causes and Treatments
- Can a Herniated Disc Cause Permanent Nerve Damage?
- How Long Does It Take a Pinched Nerve to Heal?
- Surgery versus Prolonged Conservative Treatment for Sciatica
- Osteopathic Manipulative Treatment: Muscle Energy Procedure
- Lumbar Facet Syndrome – Physiopedia
- The Connection Between Weight and Spine Disease
- The effect of intermittent diet and/or physical therapy in patients with chronic low back pain
- Dermatomes Chart: Spinal Nerves and Locations