Weekly Recovery Journal — Lumbar Disc Injury
Summery of page
Injury & Recovery Progress Report
Patient:
Date of Report: 22/08/2025 – 7:30 AM
Condition: 2 x Herniated Discs (Lumbar Spine)
Period Covered: Last 2–3 Weeks (with historical background)
Background of Injury
- Original injury sustained August 2024.
- Severe pain episodes began August–September 2024, peaking during November–December 2024, with extreme sleep deprivation (up to 5 consecutive days without sleep, even under 20 mg Valium).
- Initial treatment plan: Physiotherapy (7 months total) — provided short-term relief but plateaued after 3–4 months. Pain relief became limited, and no further healing progress was noted.
Transition in Treatment
- Due to limited physiotherapy results, patient transitioned to a combined osteopathy + chiropractic treatment model (same clinic, coordinated care).
- Treatment modalities introduced:
- Manual adjustments (front and limited back adjustments only) → side adjustments postponed to prevent further disc/nerve damage.
- Spinal decompression therapy (traction bed) → aimed at reducing nerve compression and improving mobility.
- Infrared light therapy → circulation and tissue repair.
- Hands-on manipulative therapy → broader range compared to physiotherapy.
- Treatment goal: Pain reduction, improved circulation, reduced nerve pressure, and avoidance of spinal surgery.
Notable Events in Past 3 Weeks
- Neurological Symptom – “Itching/Ants Sensation”
- After spinal adjustments ~3 weeks ago, patient developed intense deep spinal itchiness, described as “ants crawling inside spine,” unrelievable by scratching.
- Suspected cause: abnormal nerve communication/signaling between upper and lower herniated discs.
- Secondary osteopathic treatment applied → improved circulation and sensation → itching subsided and pain localized more consistently in lower back.
- Exercise / Activity Log
- Tuesday gym sessions maintained.
- Activity: 30 minutes light weights (≤10 kg) + treadmill walking.
- 17 minutes treadmill at 1.24 km → pain onset at 90 seconds (sharp left leg pain).
- Continued walking while using treadmill handrails; completed 17 minutes before intolerable pain.
- Symptoms during/after treadmill:
- Shooting pain left leg → hip → knee.
- Intermittent loss of left foot function (drop foot episodes).
- Toes (esp. 3 smallest) often fail to lift → tripping risk.
Current Symptoms
Lower Back & Nerve Pain
- Pain radiates left hip → down posterior leg → knee → left foot.
- Constant nerve symptoms in left foot (3 outer toes):
- Numbness, tingling, wet/cold sensations, burning, and loss of skin sensitivity.
- Paradoxical: skin touch feels numb, but pain signals are strong.
- Pain aggravated by lying down, walking >15 mins, or treadmill use.
Mobility
- Walking: limited, requires treadmill rail for support.
- Drop foot persists, with occasional complete toe-lift failure.
- Daily activity restricted by pain and instability.
Sleep
- Severe sleep disturbance continues:
- Average 15–90 mins sleep blocks; frequent waking due to pain.
- Positions trialed:
- Recliner with padding, pillows, blankets.
- Side-lying with support (both sides painful).
- Supine (on back) → instant escalation of pain; radiation hip → knee → toes.
- Prone (stomach) → impossible due to pain.
- Blanket/sheet weight on left foot triggers pain, cramping, burning, and numbness.
- Current strategy: staying awake longer (24–48 hrs) to force sleep.
- Despite this, max continuous sleep in last 2 weeks: 1 hr 45 mins.
Progress Compared to Prior Months
- Physiotherapy plateau → no further improvement after 3–4 months.
- Osteopathy/Chiropractic care:
- Provides broader manual techniques and decompression.
- Early signs of improvement: pain more localized to lower back instead of spreading widely.
- Circulation-related issues (e.g., itching sensation) responded well to manual therapy.
- Exercise tolerance remains low but slightly improved compared to earlier months (able to push to 17 mins treadmill vs previously unable to sustain).
- Pain levels: Slight reduction at times compared to earlier extreme episodes, but still debilitating and functionally limiting.
- Sleep: Still critical problem with minimal improvement since injury onset.
Clinical Summary
- Patient presents with two herniated lumbar discs, ongoing nerve compression with associated sciatica, neuropathic pain, and partial drop foot.
- Physiotherapy offered short-term management but plateaued.
- Osteopathy and chiropractic joint-care model currently providing alternative management with manual adjustments, decompression therapy, and infrared therapy.
- Symptoms remain severe, particularly with neuropathic foot involvement and sleep impairment.
- Surgery has been avoided so far, with conservative management ongoing.
- Current risks: fall risk due to drop foot, progressive nerve dysfunction, chronic sleep deprivation, and risk of long-term neuropathic pain.
Recommendations Moving Forward
- Continue combined osteopathy + chiropractic care (manual adjustments, decompression, infrared).
- Gradually increase controlled exercise within tolerance.
- Monitor and document foot drop episodes for neurosurgical review if worsening.
- Sleep management strategies to be readdressed (possible referral to pain clinic or neurologist).
- Maintain conservative approach as long as pain/nerve function stabilizes and avoids surgery.
Date/Time: 22 Aug 2025, 7:30 am (AEST)
Location of care: Osteopathy + Chiropractic (integrated clinic), Physiotherapy (prior)
Established diagnoses & imaging
- MRI (post-CT):
- L5/S1: Broad-based posterior disc bulge (L>R) with posterior left annular tear abutting the left S1 nerve root.
- L4/5: Left facet arthropathy with mild, non-compressive annular bulging.
- No canal/foraminal stenosis; alignment and conus normal.
- CT (earlier, 06 Nov 2024): Shallow left-posterior L5/S1 disc bulge close to the left S1 root; all other levels and SI joints normal.
- Clinical picture: Bilateral sciatica left ≫ right; episodes of neuropathic pruritus; prior greater-trochanteric bursitis; severe insomnia; intermittent left toe-lift failure (trip risk).
Current precautions: Neutral spine only, front-facing movement, ≤10 kg loads, no twisting/side-bending under load.
Interval history (last 2–3 weeks)
- Pain trend: Slight, intermittent decrease in overall pain compared with earlier weeks.
- Physio course: Benefited for ~3–4 months, then plateaued. After ~7 months total with little further gain, moved to osteopath + chiropractor for broader hands-on care.
- Current clinic modalities:
- Lumbar decompression table (distraction) → reduces perceived pressure, eases motion.
- Infrared light therapy.
- Manual adjustments: Front-facing/neutral only; side-lying adjustments deferred to protect disc/nerve while healing.
- Emphasis on circulation, movement restoration, nerve decompression.
- Neuropathic itch event (~3 weeks ago): Intense deep “ant-crawling” itch in spine after an adjustment.
- Secondary treatment to same region improved circulation; itch reduced and pain relocalized to lower back
- (consistent with nerve-root irritability rather than a skin issue).
Exercise & function (last 7 days)
- Gym (Tue a.m.): ~30 min light training, ≤10 kg, neutral spine only.
- Treadmill:17 min, 1.24 km.
- Left leg pain began ~90 sec into walking; progressed.
- Required hand rails most of session.
- Intermittent left toe-lift failure (toes don’t clear → stumble risk); slightly more controllable than prior sessions.
Sitting intolerance (current)
- Hard chair: Symptoms escalate quickly (minutes).
- Soft/cushion chair: Can tolerate ~15–20 min, then must stand/move.
- Pain path when seated: Left low back → posterior thigh/hamstring → behind knee (tight/cramp) → calf → lateral/plantar left foot → toes 5–3 with numb/cold/wet/odd sensation and burning.
- Pattern suggests load + neural tension sensitivity of the S1-weighted distribution.

Sleep & positional symptoms (current)
- Severe insomnia persists. Typical sleep is 15–30 min bouts; occasionally 1–1.5 h then wakes in pain. Even after ~48 h awake, only ~1 h 45 min sleep achieved.
- Historical peak: Early after injury, 5 days awake despite diazepam 20 mg (Nov–Dec 2024 worst months).
- Supine: Rapid escalation from left paraspinal/adjacent hip → posterior thigh → back of knee (tight, bending) → lateral foot; toes 5–3 feel numb/“wet/cold/different”; cannot tolerate sheet/blanket touching the foot; cramping/burning up the leg.
- Side-lying: Either side provokes pain on the opposite side.
- Prone: Not tolerated.
- Using recliner/blankets/pillows; variable relief.


Weight trend
- Aug 2024: 106 kg.
- ~6-month plateau: ~85 kg.
- Current: 81.9 kg (Tue, gym weigh day; measured 7 days apart from prior).
- Patient perceives slightly better mobility and modest reduction in daily spikes with lower body mass.
Assessment (this week)
- Ongoing left S1 radiculopathy with central sensitization (amplified pain/itch; severe sleep disruption).
- Intermittent toe-lift failure suggests transient dorsiflexion weakness (pain inhibition vs. L4/L5 contribution) — monitor closely.
- Sitting-provoked neural tension remains a major trigger.
- Sleep deprivation is a key amplifier of pain and daytime dysfunction.


Plan — next 2–3 weeks
A. Clinic care
- Continue decompression, infrared, and front-facing manual care as tolerated.
- Keep side-lying manipulation on hold until symptoms are more stable.
- Add graded neural mobilization (“sliders”) for sciatic/S1 within pain-free range.
B. Exercise
- On flare weeks, swap treadmill for upright exercise or pool walking to reduce heel-strike neural load.
- If treadmill used: intervals (1–2 min easy walk / 1–2 min rest), stop at first motor change (toe catch/drag).
- Maintain ≤10 kg, symmetrical, front-facing patterns; tempo 3-1-3; progress by next-day ≤3/10 rule.
C. Sitting & posture
- Micro-breaks: Sit ≤10–15 min, then stand/walk 2–3 min.
- Seat setup: Lumbar roll or wedge, slight hip opening (mild recline), feet flat; avoid long slump.
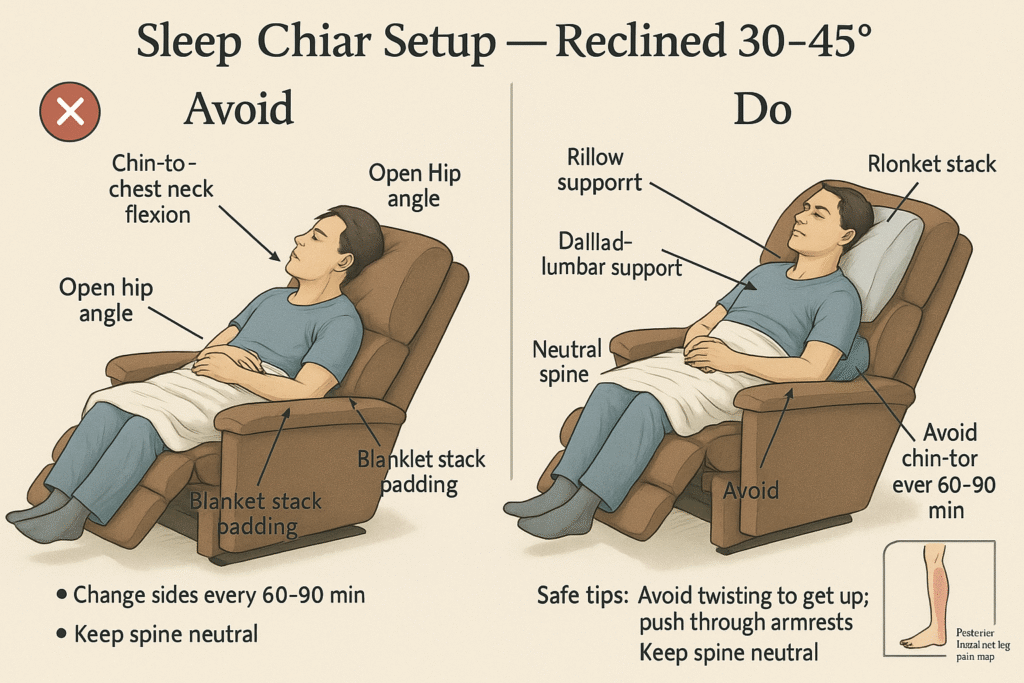
D. Sleep strategy
- Prefer 30–45° reclined or side-lying with knee pillow; avoid full supine.
- Discuss with GP: a night-time neuropathic pain agent (e.g., amitriptyline/nortriptyline, duloxetine, gabapentin/pregabalin)
- to improve sleep and dysesthesia. Avoid routine benzodiazepines.
- Heat pre-bed for guarding; brief ice for sharp flares.
E. Escalation / safety
- Urgent review for: progressive weakness (true foot drop), saddle anesthesia, or new bladder/bowel changes.
- If toe-lift failures persist or worsen, request focused neuro exam, consider EMG/NCS, and updated lumbar MRI per clinician judgment.
F. Tracking & education
- Daily log: pain (0–10), sleep minutes,
- minutes walked, sitting tolerance.
- Reinforce neutral-spine mechanics,
- no twisting/side-bending under load, and pacing.
Patient-friendly summary
I’ve had small improvements in pain at times the last few weeks. Physio helped for months but then stalled,
so I moved to a clinic where an osteopath and chiropractor treat me together.
They’re using a decompression bed, infrared, and gentle front-facing adjustments (no side adjustments yet).
A few weeks ago I had a horrible deep spinal itch after treatment; a follow-up session settled it,
Where the pain stayed more in my lower back after treatment.
This week I trained gym light for ~30 minutes and walked
17 minutes (1.24 km) on the treadmill.
Pain down the left leg started at 90 seconds.
I used the rails and kept going until I couldn’t.
Sometimes my toes don’t lift properly,
but I controlled it a bit better than before using rails to help take some weight when walk
Sitting sets off my pain:
hard chairs are worst; on a cushion I last 15–20 minutes before I have to get up.
The pain runs from my left low back down the hamstring,
behind the knee, into the calf, and the
outside/toes 5–4-3 feel numb/cold/wet/different with burning. 5 being start little toe
Sleep is still poor — often minutes to an hour at a time. I’m adjusting positions, using a wedge/lumbar roll,
My weight has gone from 106 kg to 81.9 kg,
which helps a little with mobility.
What foot drop is
Foot drop means it’s hard to lift the front of your foot (dorsiflex), so the toes drag
or you compensate with a high “steppage” gait (lifting the knee/hip extra to clear the ground).
It’s a symptom of an underlying nerve/muscle problem, not a disease by itself. Mayo ClinicNINDS
Classic causes
- Peroneal (fibular) nerve injury/compression at the outside of the knee (very common). Cleveland ClinicGPnotebookBMJ Evidence-Based Medicine
- Lumbar radiculopathy, especially L5 nerve root (often from a disc issue) — this one lines up with back/leg pain patterns. Cleveland ClinicPhysiopedia
- Less common: stroke or other brain/spinal disorders, motor neuron disease, severe neuropathies, trauma. Mayo Clinic
Typical symptoms & gait
- Toes don’t lift when you swing the leg → toe catch, tripping, or foot “slap” when the heel strikes.
- You may hike the hip/knee (steppage gait) so the toes clear.
- Numbness can accompany it, depending on which nerve/root is involved. Spine-healthDoveMed
How this relates to your scans/symptoms
- Your imaging shows L5/S1 disc bulge with annular tear abutting the left S1 root, plus L4/5 facet arthropathy.
- Foot drop itself is classically L5,
- while your toe numbness in toes 3–5 and lateral foot screams S1 — so you may have
- S1 sensory irritation with intermittent L5-type dorsiflexion inhibition (pain-guarding) or a
- contribution from the peroneal nerve.
- A focused neuro exam can separate these. PhysiopediaCleveland Clinic
How doctors confirm it
- Neuro exam: strength of tibialis anterior/extensor hallucis (L4–L5), sensation maps, reflexes.
- EMG/Nerve conduction to tell L5 root vs peroneal nerve problem.
- Imaging if red flags or progressive weakness. Cleveland Clinic
Treatment (depends on cause)
- Treat the driver: lumbar care for radiculopathy (injections/surgery only if needed),
- or relieve peroneal nerve compression. Cleveland Clinic
- Physio/gait training and dorsiflexor strengthening; sometimes neuromuscular stimulation. Verywell Health
- AFO brace short-term to stop toe drag and falls;
- surgical tendon transfer only for persistent cases. Cleveland ClinicMayo Clinic
When to escalate urgently
- Worsening weakness, new true foot drop
- you can’t overcome, saddle numbness, or bladder/bowel changes → urgent medical review. (Safety first.)

Neck Pain Symptom Summary
Primary Complaint
- Neck and upper back pain with radiating symptoms.
Pain Pattern
- Origin: Left shoulder area.
- Radiation:
- Moves from shoulder into the space between the shoulder blade and spine.
- Extends up the side of the neck.
- Travels further into the left side of the head/temple region.
Characteristics
- Pain appears nerve-related and radiating, not isolated to one spot.
- Affects shoulder → scapula → cervical spine → side of neck → head.
- May suggest cervical spine involvement (nerve compression or disc issue) or muscle/nerve irritation along the cervical-thoracic junction.
Impact
- Contributes to neck stiffness.
- Can trigger headache-type pain at the left temple.
- May overlap with existing lower back/spine nerve pain patterns, indicating multiple spinal segments under stress.
Prepared by: Brentdee
For: Treating GP / Osteopath / Chiropractor / Physiotherapist



